KNOW YOUR OPTIONS
If you have dense breasts (categories C and D), mammography alone may not be enough for you.
In addition to mammography, there are more supplemental screening options than you might think.
The way to find out your breast density is to get a mammogram
or read a recent mammography report.
If you don’t have dense breasts, a mammogram will find 98% of cancers.
If you DO have dense breasts, a mammogram will find LESS THAN 50% of cancers.[2,3,4]
“If I see no signs of cancer on a mammogram in a woman with dense breast tissue guidelines require breast radiologists like me to issue a report that the exam is negative. But my confidence in that negative assessment is shaken because I know there is a possibility that cancer could be present but I can’t see it. This causes me to wonder–is this woman really ok? What extra imaging can I offer to prevent her from returning in the future with a palpable cancer?”
-Dr. Matthew Covington, University of Utah

Which screening option is right for YOU?
Helpful Definitions
Find Rate: The number of cancers found per 1000 women screened
Recall Rate: The percentage of time you will be called back for more imaging
False Alarm: The percentage of time cancer will be suspected, biopsy taken, but NO cancer found – unnecessary biopsy
Best For: women of screening age with Breast Density A or B
Availability: Widely Available
Find Rate: 1.8 – 3.2 /1000 women screened[5,6,7,8]
Recall Rate: 10.3% of women screened[9]
False Alarm: 50-60% of patients over 10 years, or 7-12% of patients per year[9]
COST & COVERAGE
- Covered by most insurance companies, Medicare & Medicaid.
- Uninsured patient price ranges $80 – $120, with an average of $102. See More
Since September 2010, the Affordable Care Act has required all new health insurance plans to cover screening mammograms every 1-2 years with NO out-of-pocket costs (copays or co-insurance) for women ages 40+.

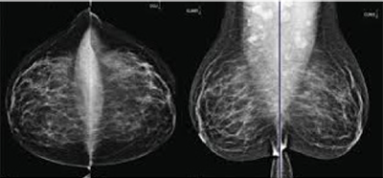
A conventional or 2D mammogram takes a single image of your breast with each exposure.
- Exposure to low level of radiation
- Frequently not accurate in dense breast tissue
- Dense tissue, scar tissue, and implants can negatively affect results
- May lead to additional testing
- Can’t detect ALL cancers – especially in dense tissue
3D Mammogram
(DBT – Digital Breast Tomosynthesis)
Best For: women of screening age with breast density C & D
Availability: Increasingly Available
Find Rate: 1-2 per 1000 women screened increase over standard mammography[10]
Recall Rate: 3D reduces call backs compared to 2D[11]
False Alarms: 3D reduces false positive rate compared to 2D[12]
COST & COVERAGE
- Uninsured patient price ranges $143 – $413. Learn More
- Insurance coverage for 3D mammograms varies greatly. You should check with your carrier to see what their policy is.

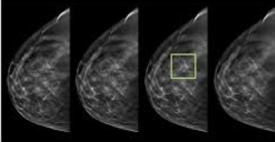
A 3D mammogram takes multiple images of your breast as the machine moves in an arc. A computer then assembles these into 3-dimensional images that allows the doctor to look through the breast in “slices” or layers rather than just a single image.
- Exposure to low level of radiation
- May lead to additional testing
- Can’t detect ALL cancers – especially in dense tissue
Molecular Breast Imaging “MBI”
Best For: women with dense breast tissue (C or D), but no other risk factors, OR if you’re high risk but can’t undergo MRI
Find Rate: 9.3 per 1000 additional cancers found when added to 3D mammography (tomosynthesis) in women with dense breasts[28]
Recall Rate: 7.6% of women recalled[15]
False Alarms: 6.4%[15]
COST & COVERAGE
- The typical out-of-pocket cost for MBI is about $450.
- Medicare and Medicaid will cover MBI.
- Insurance coverage for MBI varies widely. Check with your provider regarding coverage.

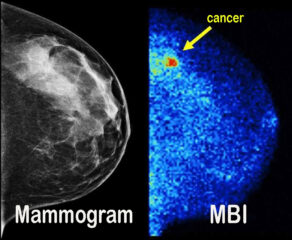
MBI is an advanced screening technology typically used in addition to mammography. MBI uses a tracer that “lights up” areas of cancer in the breast. These areas light up because breast cancer cells absorb more of the radioactive substance than normal cells.
- low dose radioactive injection
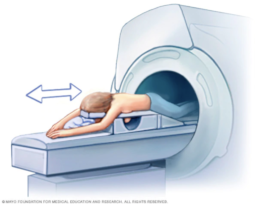
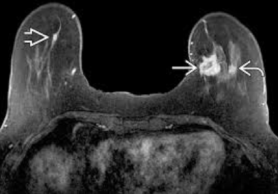
Magnetic Resonance Imaging “MRI”
Best For: high risk patients
Availability: Widely Available
Find Rate: 16 per 1000 additional cancers found when added to mammography[16]
Recall Rate: 26% [17]
False Alarms: 24% [18]
COST & COVERAGE
- The average cost of an MRI is about $1,084.
- Some insurance plans will cover screening MRIs if you can prove that you are at high risk for developing breast cancer.

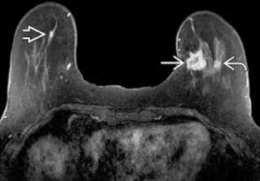
Breast MRI (magnetic resonance imaging) is an advanced screening modality that uses radio waves, strong magnets, and an injected contrast agent to make detailed pictures of the inside of your breast. MRI is used as an advanced screening technology in addition to mammography.
- NO radiation risk
- Possible reaction to the contrast used
- High rate of false positives
- Can’t be used for those with metal in their body, with compromised renal systems, or claustrophobia
Abbreviated Magnetic Resonance Imaging
“Abr. MRI”
Best For: Women with dense breast tissue categories C or D
Availability: Known Abbreviated MRI Locations
Find Rate: 10 additional cancers found when added to mammography[19]
Recall Rate: 7.5%[19]
False Alarms: not available
COST & COVERAGE
- There is currently no insurance for Abr. MRI.
- Only self pay options are currently offered — see Known Locations for estimated costs.
Breast MRI (magnetic resonance imaging) is an advanced screening modality that uses radio waves, strong magnets, and an injected contrast agent to make detailed pictures of the inside of your breast. Abr. MRI offers faster imaging time using fewer images than Full MRI. Abr. MRI is used as an advanced screening technology in addition to mammography.
- NO radiation risk
- Possible reaction to the contrast used
- Can’t be used for those with metal in their body, with compromised renal systems, or claustrophobia
Handheld Ultrasound
Best For: very young women, pregnant women, and for additional screening
Availability: Widely Available
Find Rate: Finds 2-2.7 more cancers per 1000 women with dense breasts, increase over standard mammography[13]
Recall Rate: 10.7% (increases recall rate)[14]
False Alarms: False positives are more common, >20%[14]
COST & COVERAGE
- Uninsured patient price is typically $250.
Most insurance plans do NOT cover a breast screening ultrasound.

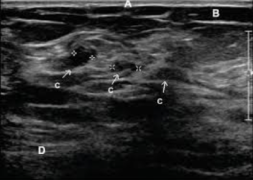
Handheld Ultrasound is a supplemental screening technology used in addition to mammography. Ultrasound image of the breast is performed by a doctor or tech using a handheld probe to scan breasts.
- NO radiation risk
- Requires a highly skilled operator
- Has a lot of false positive findings
Automated Breast Ultrasound “ABUS”
Best For: very young women, pregnant women, dense breast tissue (C or D), high risk patients that cannot undergo breast MRI
Find Rate: 2-2.7 per 1000 additional cancers found when added to mammography[13]
Recall Rate: 10.7% (increases recall rate)[14]
False Alarms: False positives are more common, >20%[14]
COST & COVERAGE
- Often covered by insurance.
- Out-of-pocket co-pay can range from $0 to $147.


ABUS is an ultrasound image of the whole breast that is automated and performed by a machine. It is used as supplemental screening in addition to mammography.
- NO radiation risk
- Minimal breast compression
Contrast Enhanced Spectral Mammography “CESM”
Best For: may benefit women with an intermediate to high lifetime risk of breast cancer and women with dense breast tissue
Find Rate: 13 per 1000 in addition to mammography[20]
Recall: data unavailable
False Alarms: data unavailable
COST & COVERAGE
- Not typically covered
- Check with your insurance carrier

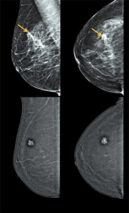
A CESM is an advanced screening technique that is a mammogram that uses a type of contrast injection to create a picture of the breast tissue by combining two images: one showing contrast injected, the other a regular mammogram.
- May have reaction to contrast used
- Low dose of radiation
Breast Thermography
 IMPORTANT: The FDA warns Thermography should NOT be used in place of Mammography to detect, diagnose, or screen for Breast Cancer.
IMPORTANT: The FDA warns Thermography should NOT be used in place of Mammography to detect, diagnose, or screen for Breast Cancer.
Read More
Only limited data is available; only 1 study on 63 subjects from 2011: click to view more on the study.
COST & COVERAGE
- Be sure to confirm cost before you have the procedure.
- Most insurance plans do NOT cover it.
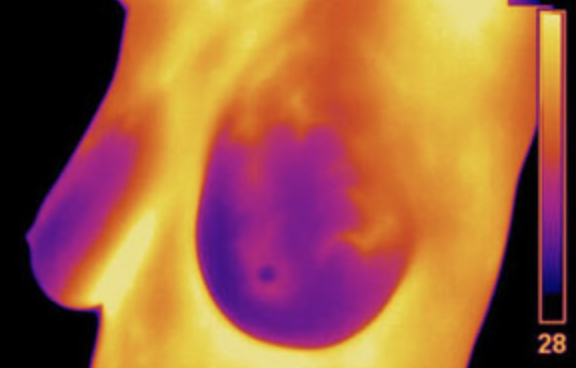

Thermography, also called thermal imaging, uses a special camera to measure the temperature of the skin on the breast’s surface. It is non-invasive test that involves no radiation.
Thermography is based on two ideas:
• Because cancer cells are growing and multiplying very fast, blood flow and metabolism are higher in a cancer tumor.
• As blood flow and metabolism increase, skin temperature goes up.
Thermography has been available for several decades, but there is no evidence to show that it’s a good screening tool to detect breast cancer early, when the cancer is most treatable.
If you have been told you have dense breast tissue (C or D) and are concerned, talk with your doctor. Depending on your risk factors and personal preference, together you can decide if additional screening tests are right for you.
Insurance
If insurance does not cover a screening, you can “self-pay.”
Roadblocks
It’s not always easy getting the screening you want.
Resources
Review scripts and links to help secure your preferred screening.









 Carmen West is a Senior Global Human Capital & Change Transformation Professional.
Carmen West is a Senior Global Human Capital & Change Transformation Professional.






